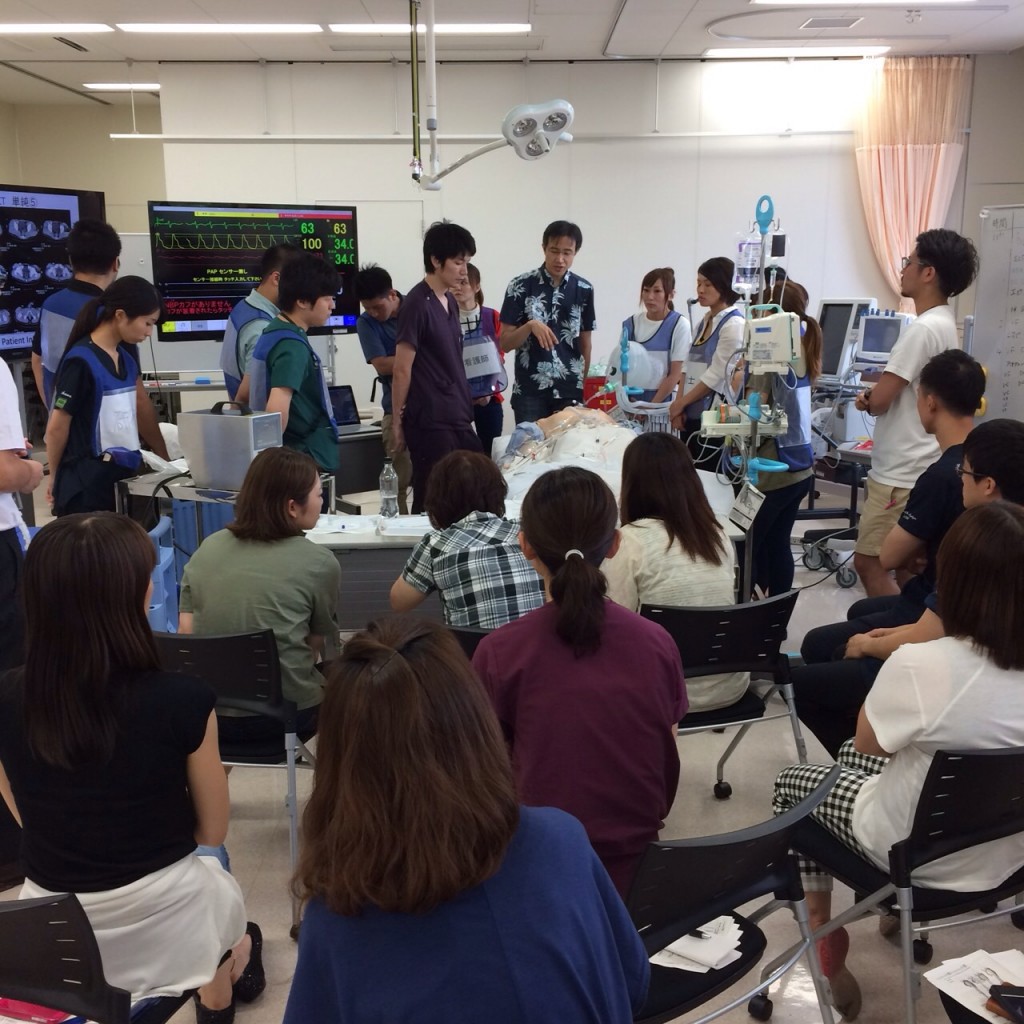
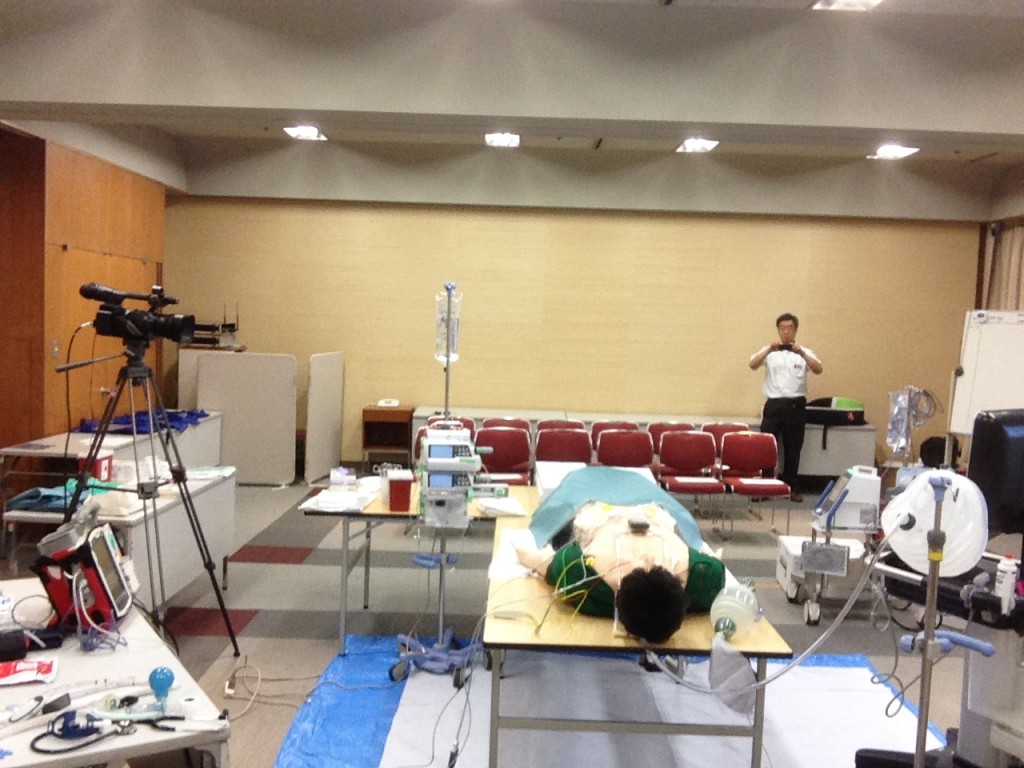
On July 26, SimMarathon in Okinawa clinical simulation center was done as scheduled. This center’s nickname is “Chura-Sim”. “Chura” means “beautiful” in Okinawan dialect. As it is, this center is very beautiful and well-equipped for training.
This time, all participants belong to a certain private hospital near this center.
An experienced doctor Mito who is a friend of mine since 2001 is in charge of emergency room of the hospital and invited me as a director of this simulation seminar.
More than 20 people joined and completed 8 scenarios as follows.
I really appreciate this remarkable facility and Dr Mito’s enthusiasm about simulation education.
In addition to holding seminar, I went to Okinawa’s sacred spot called Seifa-Utaki and then Syuri-Castle. Of course I enjoyed lots of local yummy foods.
44 M
CC; burn
Dx; large burn by explosion, face to leg, TBSA 40%
PH; n.p.
Tx; Airway control, fluid resuscitation by Parkland formula, wound care etc
67 M
CC; altered consciousness
Dx; Hyperkalemia,Acute Pancreatitis(alcoholic) with ARDS by CECT, severe shock
PH; alcoholics
Tx; Calcium iv, massive fluid resuscitation, ABx, intubation, low tidal volume ventilation for ARDS
60M
CC: lt.hemiparesis, altered consciousness
Dx: AAD(Stanford A), dissection of 3 branches from aortic arch, seizure
Tx; intubation, CECT→ope
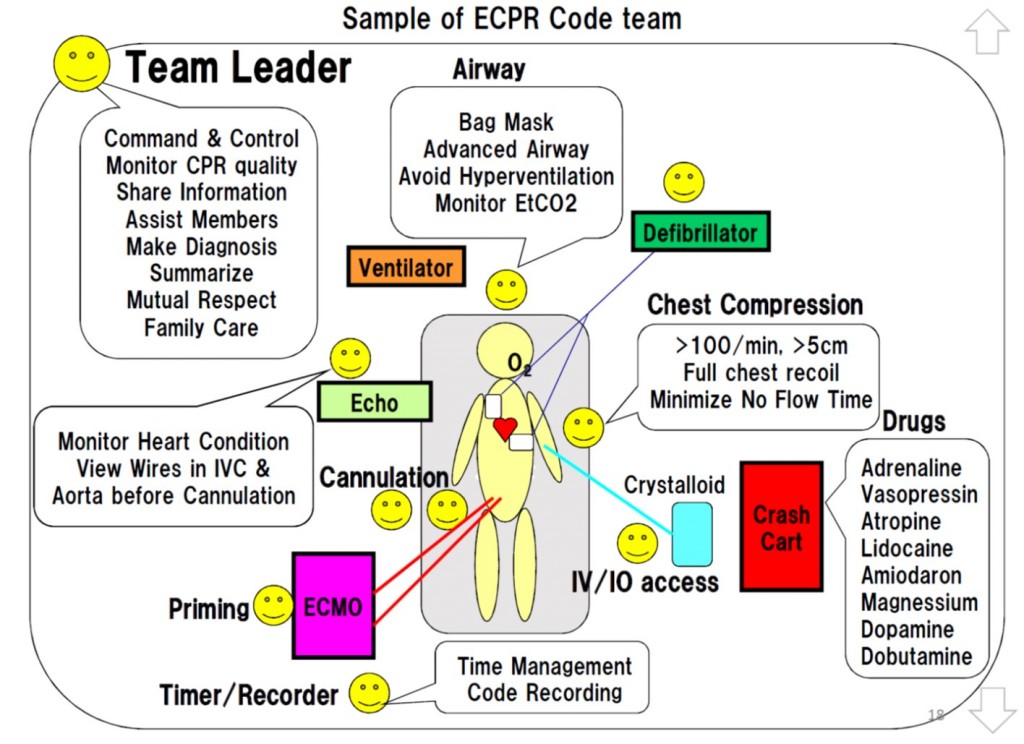
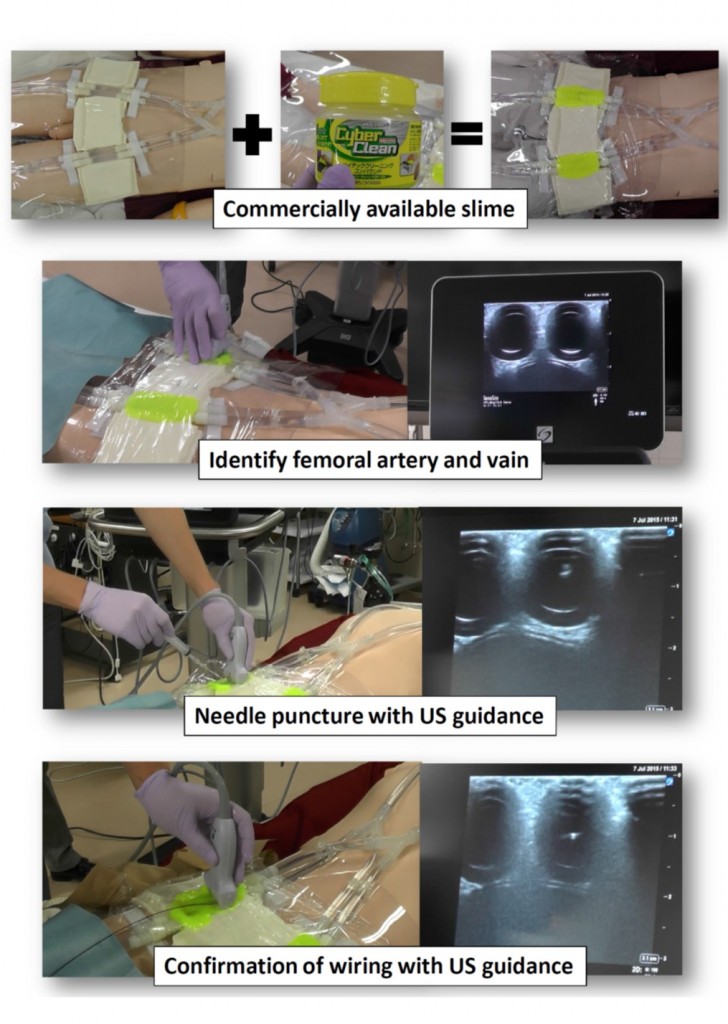
20 M
CC; syncope, LOC→gasping, VF
Dx; Idiopathic VF, persistent VF
PH; WPW syndrome
Tx; DC many times/adrenaline/amiodarone/intubation → ECPR(PCPS) → rhythm conversion → CT(full body)& CAG, TTM
20M
CC; death-leap from 5th floor of an apartment, facial injury, leg deformation
Dx; hemorrhagic shock due to pelvic fracture, lt femor fracture and other limb fractures
PH; isolating himself from society
Tx; intubation/blood transfusion/FAST and FACT→TAE
53 M
CC; pyrexia, rt leg swelling,pain & erythema, consciousness down
Dx; NSTI with gas of rt. leg, septic shock/DIC
PH; untreated DM
Tx; EGDT, ABx, CECT, not only debriedmant but amputation needed for source control
50 M
CC; syncope, dyspnea, cyanosis
Dx; massive PE/DVT→syncope/shock
PH; overweight
Tx; intubation/catecholamine→VA-ECMO(PCPS)→CECT
52F
CC; severe hypoxemia, orthopnea
Dx; AHFS CS1+2, MR (MVP)
PH: HT, post Y-grafting for AAA
Tx; intubation, nitrate, diuretics