I’ve been enthusiastic about providing ECMO simulation for these several years.
In 2013, I created a half-day ECMO sim at Simulation Center of Tohoku University Hospital in Sendai and I’ve been holding this simulation almost every single month for ECMO practitioners.
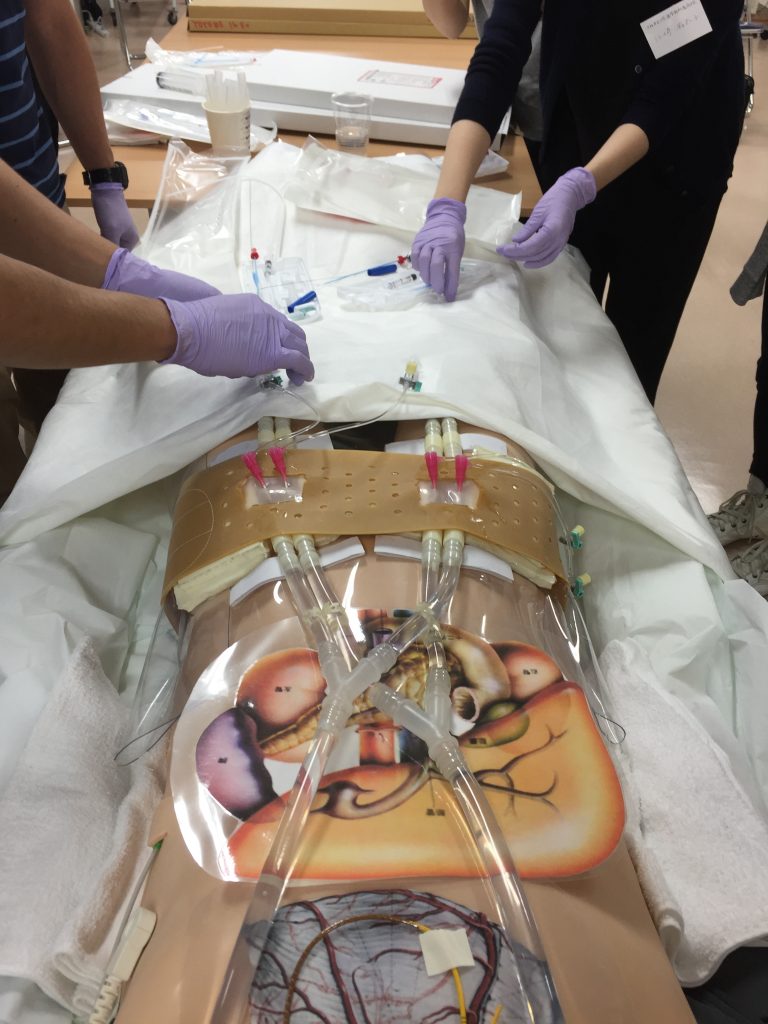
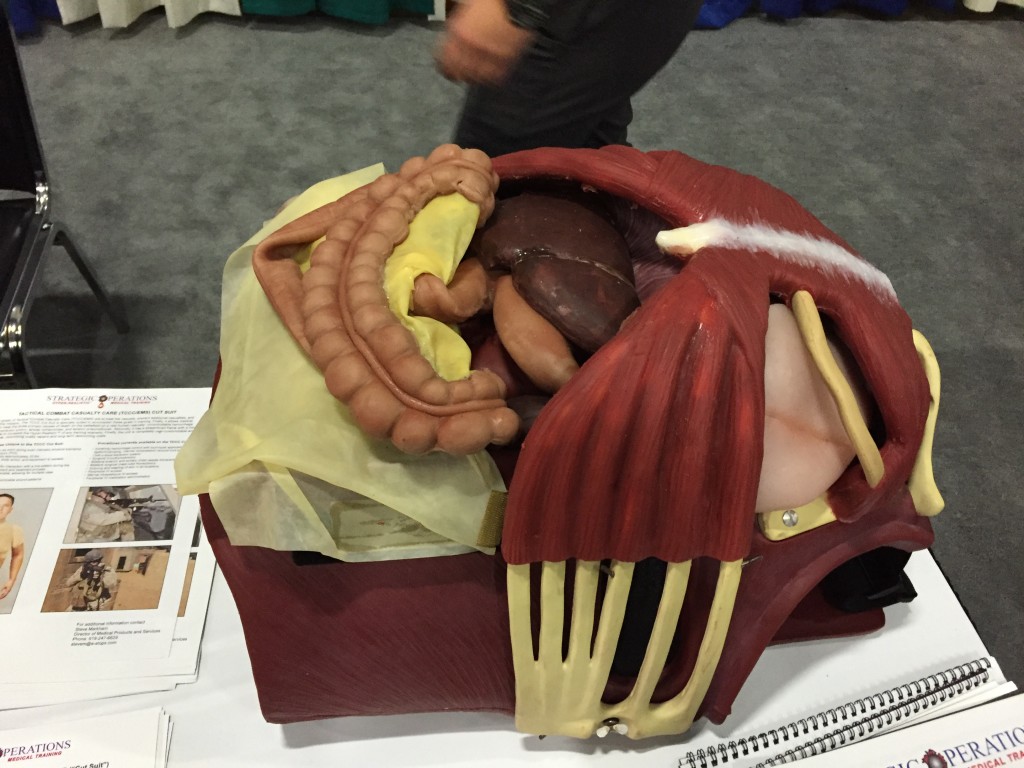
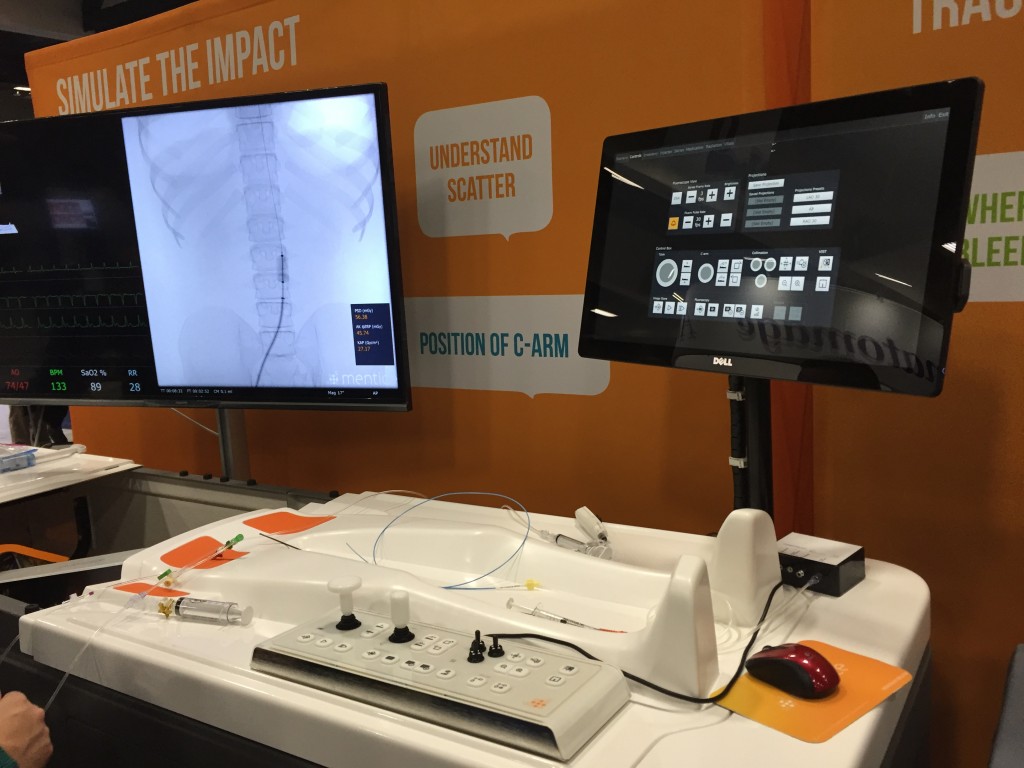
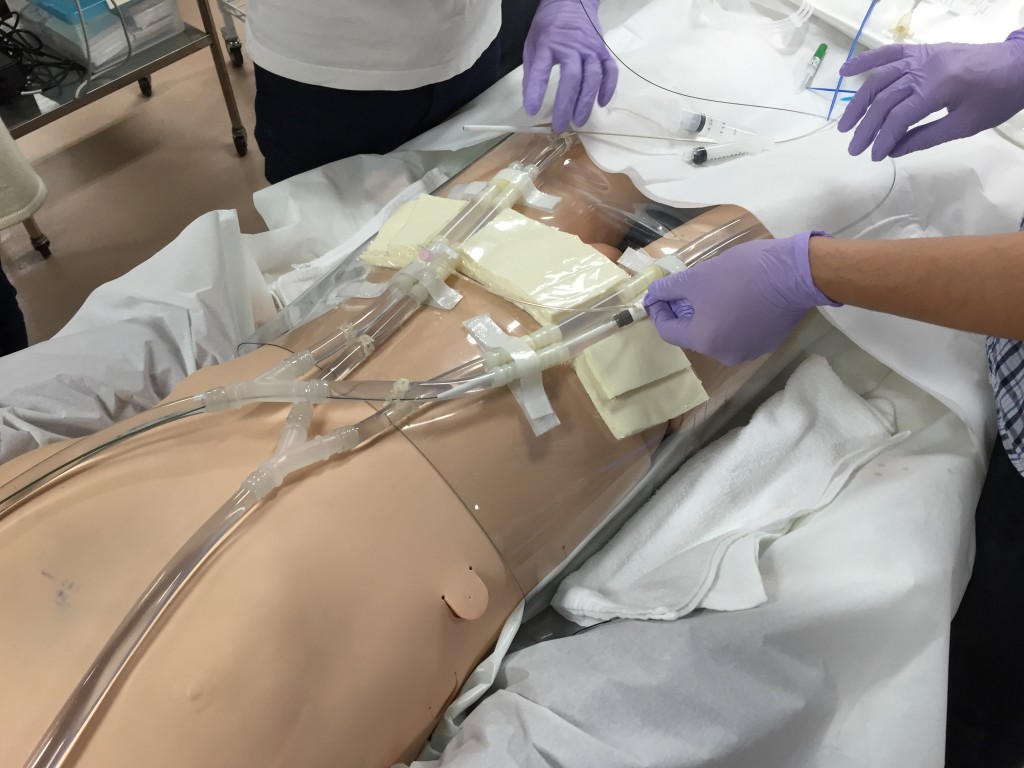
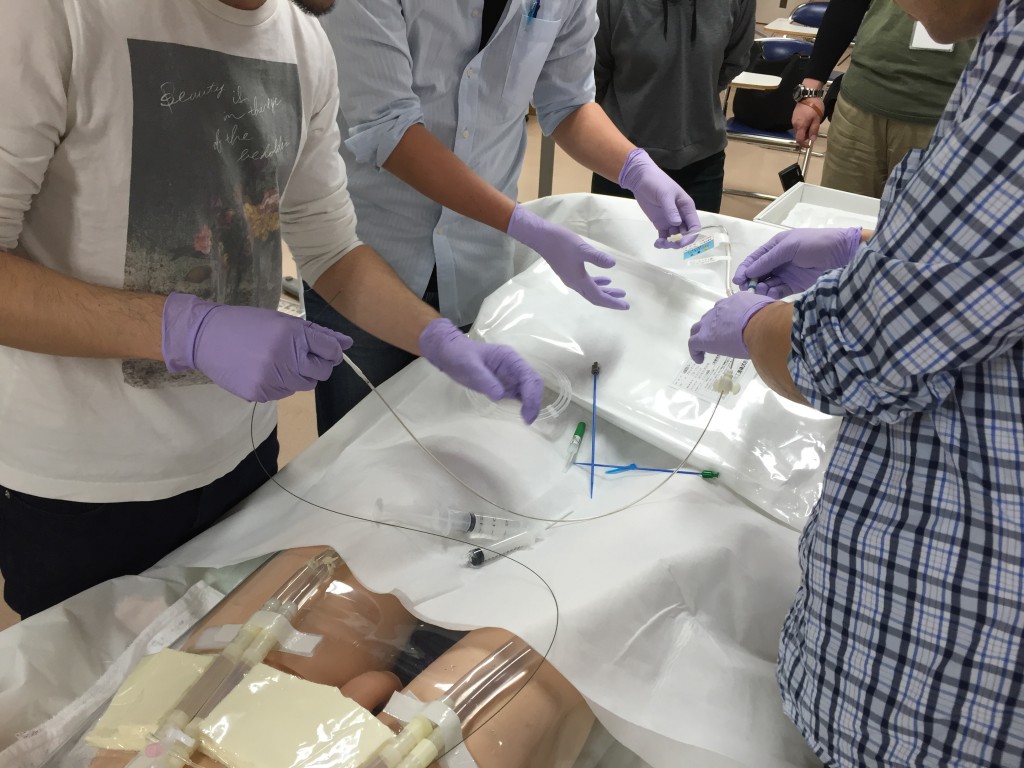
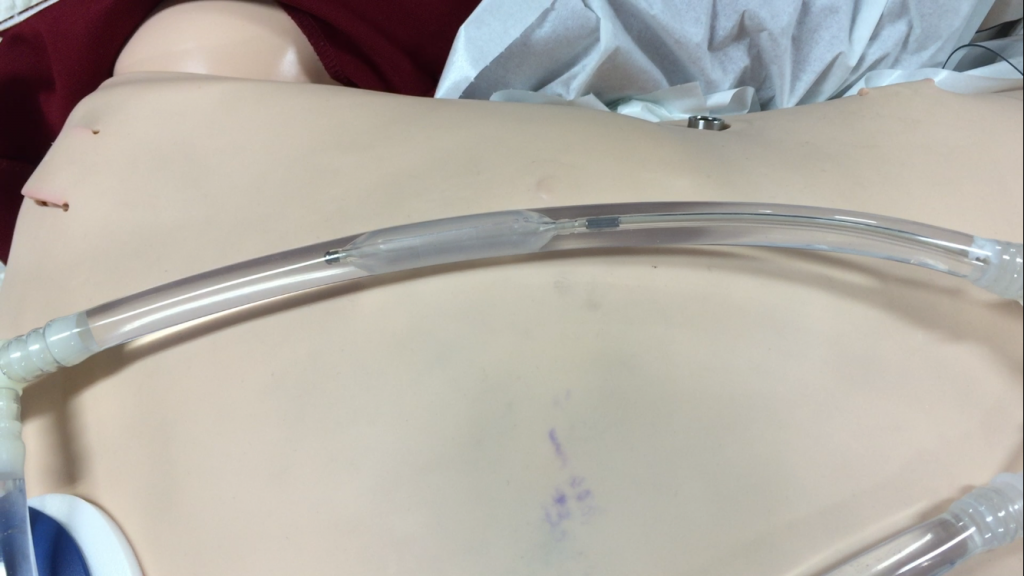
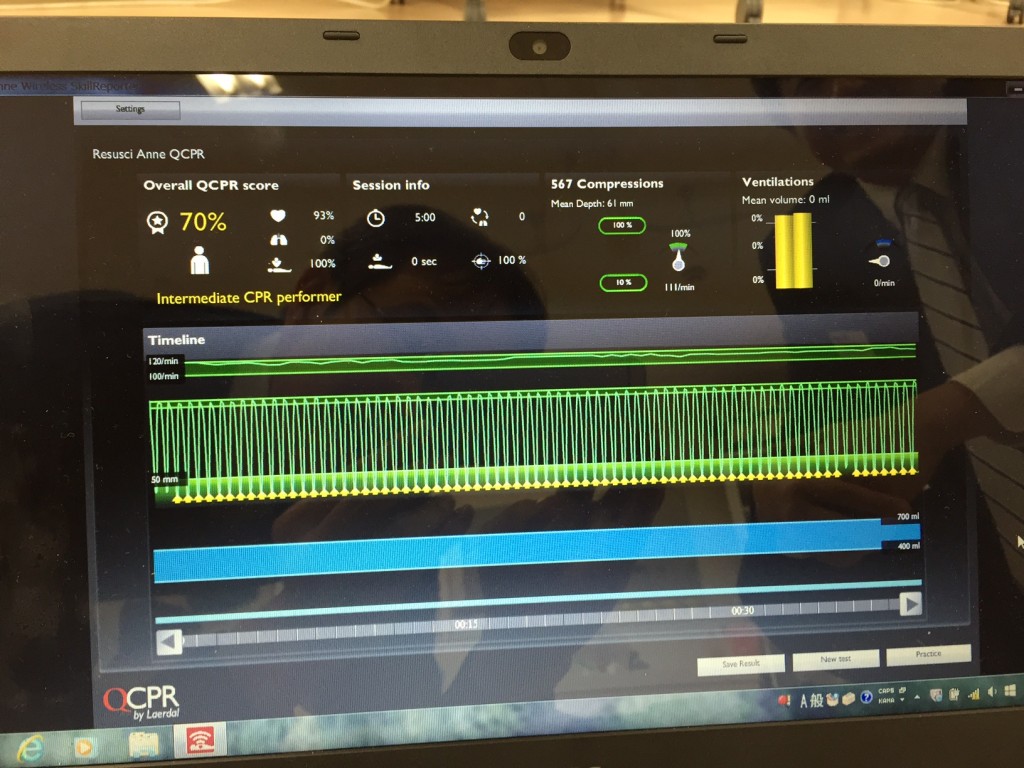
This is focused on VA-ECMO at Emergency Department. ELSO guideline was used as a reference. In order to make it possible for learners to practice ECMO cannulation and initiation of ECMO, I developed a low cost imitated vascular model named “Endo-Circuit”.
Recently I published a research about the long term efficacy of my ECMO simulation with the “Endo-Circuit” on peer-reviewed journal; “Acute Medicine & Surgery”, doi: 10.1002/ams2.236
My research revealed that many ECMO practitioners in Japan have some sort of PROBLEMS and FEARS about ECMO practice before simulation and then they have gotten some positive change in their knowledge, skills and attitudes after simulation. Since this research was only based on their retrospective self-evaluation, it’s unsure that their actual ECMO practices have been changed and lead to safer management. However some of their answers show that their usage of ultrasound for needle puncture and confirmation of guidewire placement during cannulation increased than before.
Even though the model is less expensive and imperfect in terms of anatomy of cardiovascular system, their evaluation about the circuit as a training model is relatively high. In order to keep quality of ECMO practice, this kind of simulation should be provided constantly.
In addition to my ECMO simulation, Japanese Circulation Society (JCS) and Japanese Resuscitation Council (JRC) had developed a one-day post cardiac arrest syndrome (PCAS) care training course in 2014 including ECMO skill training with “Endo-Circuit” and added an integrated ECPR team simulation in 2016.
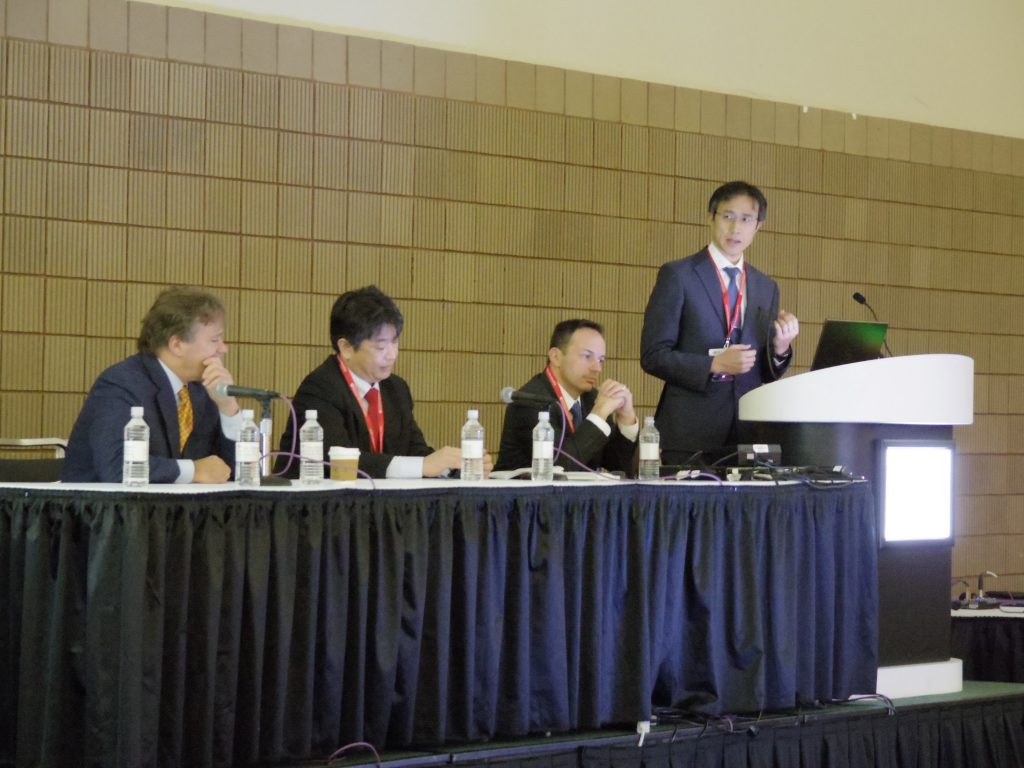
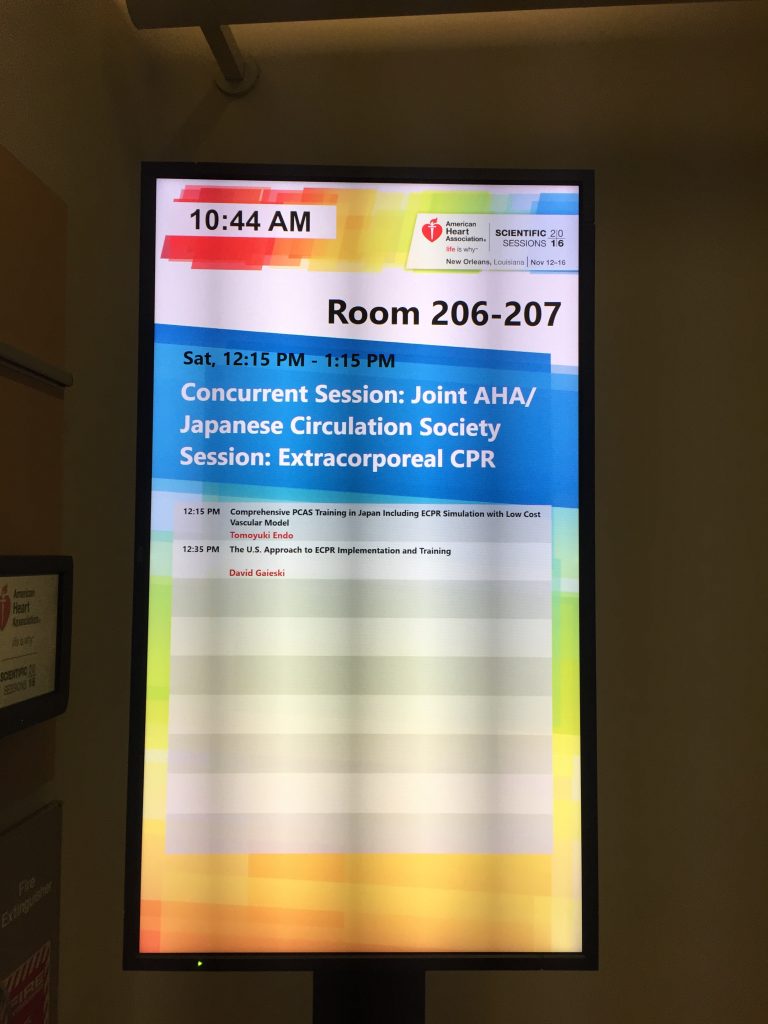
Fortunately I got a fantastic opportunity to talk about JCS PCAS care training with my original training model at AHA/JCS Joint Session of Resuscitation Symposium in 2016 in New Orleans.
On Nov 12, I gave a 20-min presentation about our special educational experience including ECPR video for enthusiastic ECMO/ECPR providers attending the session. I had practiced my presentation a lot before the session and indeed my presentation was successful in terms of letting them know our project. There were some respected resuscitation researchers at the session. It was an amazing experience. My counterpart was Dr. David F. Gaieski and he talked about current US status of ECPR implementation and training. There were some hot discussions related to this topic.
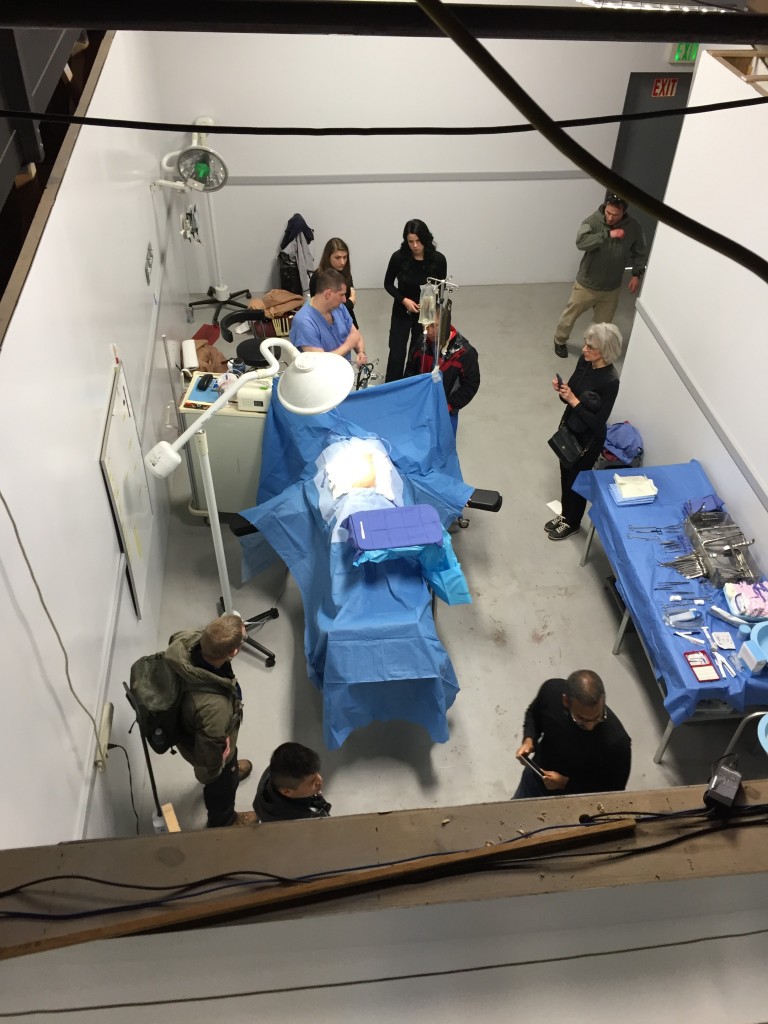
On Nov 13-14, I did a ECPR cannulation Demo at JCS Booth in Exhibition Hall. Several attendees enjoyed my training model and some gave me compliments about it. I spent such a fantastic time in New Orleans.
ECPR is always challenging in terms of cost, human resources, time sensitivity, difficulty of cannulation, combination with TTM, uncertainty of heat and neurological recovery etc.
To make ECPR validated, I believe the standardized training including cannulation practice should be held for every advanced resuscitation provider repeatedly like BLS/ACLS.
I want to stay in touch with current enthusiasm about ECMO/ECPR and keep providing decent simulation seminars for practitioners.